Strategies for Pediatric Asthma Management: A Specialist's Guide for 2025
The Global Pediatric Asthma Challenge
Pediatric asthma remains the most prevalent chronic respiratory condition affecting children worldwide, with approximately 300 million current cases and a projected rise to 400 million by 2025. It requires a nuanced approach from specialists who understand the unified airway. For otolaryngologists, allergists, and pulmonologists, effective management extends beyond prescription; it involves equipping parents with evidence-based strategies and a deep understanding of their child's condition. The following five strategies, supported by recent research, are critical for optimizing outcomes.
Mastery of Inhaler and Spacer Technique Through Validated Teach-Back
The Evidence: Proper medication delivery is the cornerstone of effective asthma control, yet studies consistently show that up to 70-80% of patients use their inhalers incorrectly, significantly reducing drug deposition and therapeutic efficacy. For pediatric patients, this challenge is compounded by developmental factors that vary with age and cognitive ability.
Specialist Application:
- Implement Demonstration & Validation: Move beyond verbal instruction. Perform live demonstrations using placebo devices and implement a mandatory "teach-back" method where parents and children demonstrate their technique before leaving the clinic.
- Age-Specific Device Selection: Individualize devices based on age and ability.
- Children under 4: Masked valved holding chambers with face masks
- Children 4-8: Transition from masks to mouthpieces while monitoring technique
- Children 8+: Consider dry powder inhalers or metered-dose inhalers with spacers based on preference and ability
- Address Resistance: For resistant young children, discuss techniques like positive reinforcement and mask desensitization. For adolescents, consider digital health tools like smartphone apps with AI-based technique analysis to ensure ongoing adherence.
Trigger Identification & Environmental Control
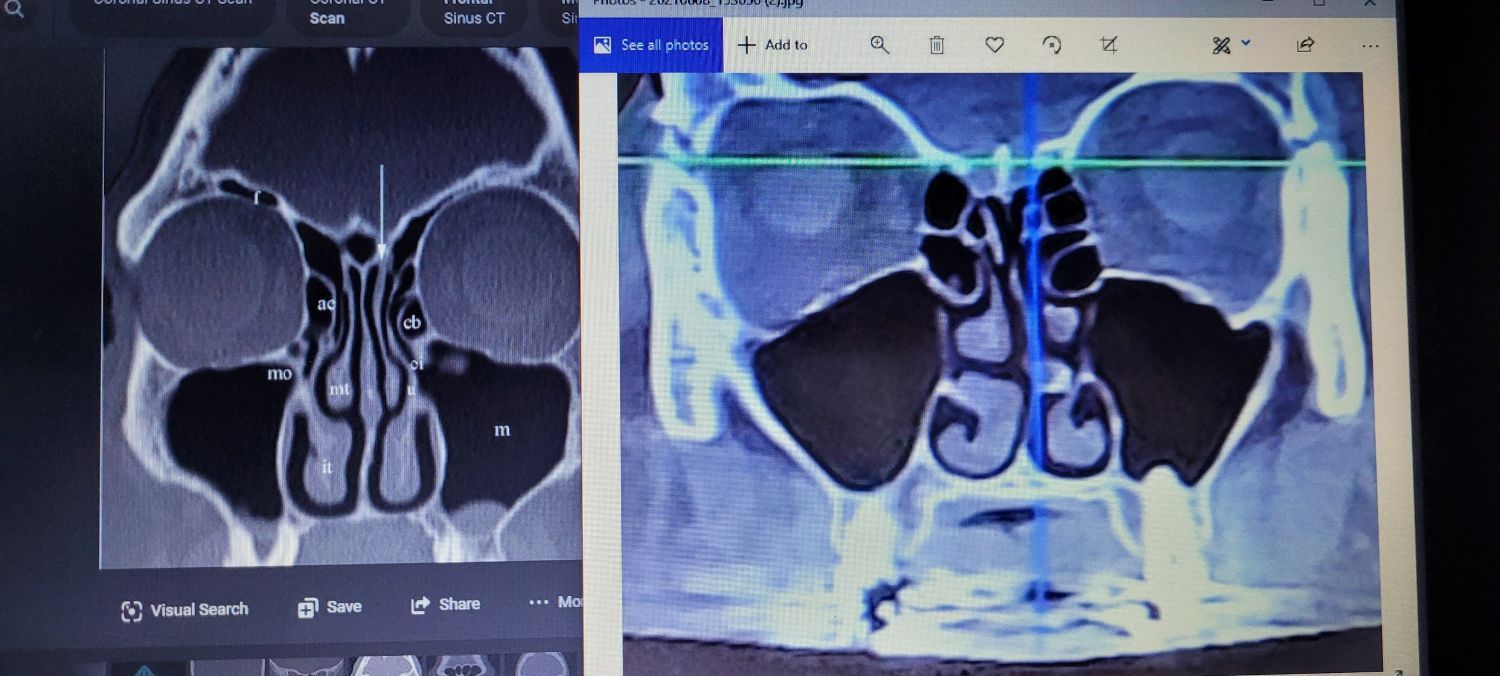
The Evidence: The unified airway paradigm recognizes that upper and lower airway inflammation are intrinsically linked, with rhinitis and sinusitis significantly impacting asthma control. A 2025 study in JAMA Pediatrics demonstrated that environmental trigger exposure accounts for up to 80% of asthma exacerbations in urban children, with complex interactions between allergens, pollutants, and viral infections. Furthermore, a Cochrane review confirmed that multifaceted environmental interventions reduce exacerbations by 37%.
Specialist Application:
- Conduct a Structured Environmental History: Systematically identify aeroallergens, pollutants, and irritants. Emphasize the role of uncontrolled sinonasal inflammation in lowering the bronchial threshold for reactivity.
- Advocate for Targeted Interventions: Recommend specific actions based on triggers:
- HEPA Air Filtration: To reduce particulate matter and allergens
- Integrated Pest Management: Preferable to chemical pesticides for cockroach and rodent control.
- Humidity Control: Maintain 40-50% indoor humidity to reduce mold and dust mite growth.
- Dust-Proof Bedding: Encasements for mattresses and pillows are proven to reduce exposure.
- Discuss Outdoor Air Pollution: Counsel families on monitoring the Air Quality Index (AQI) and creating "clean air spaces" at home, especially in the child's bedroom.
Implementation of Personalized, Proactive Monitoring Protocols
The Evidence: Significant socioeconomic and racial disparities exist in asthma outcomes. CDC data shows prevalence is highest in non-Hispanic Black (11.6%) and American Indian/Alaska Native (12.3%) children compared to non-Hispanic White children (5.5%). Proactive, risk-stratified follow-up is essential to address these disparities.
Specialist Application:
- Risk-Stratified Follow-Up:
- High-risk patients (recent exacerbation, poor control, significant comorbidities): Two-to-four-week follow-up after adjustment
- Moderate-risk patients: Four- to eight-week follow-up until improved control
- Well-controlled patients: Three-to six-month, routine follow-up
- Utilize Standardized Tools: Employ validated control questionnaires (c-ACT/ACT) and spirometry at routine visits to objectively assess control.
- Screen for Social Determinants of Health: Actively ask about barriers to care, including medication cost, housing quality (e.g., mold, pests), and food security. Leverage community health workers where available.
Provision of Curated Resources and Facilitation of Interdisciplinary Care
The Evidence: The complexity of pediatric asthma, particularly severe phenotypes, demands collaboration. Platforms like the Snot Force Alliance model this interdisciplinary approach, bringing together otolaryngologists, allergists, and pulmonologists to address the unified airway.
Specialist Application:
- Provide Condition-Specific Written Action Plans: Give parents a written asthma action plan that uses a clear "stoplight" system (green, yellow, red zones) to guide daily management and emergency response.
- Offer Authoritative Resources: Direct parents to reputable organizations for booklets and digital content that explain the integrated nature of airway health.
- Refer Early and Often: The 2025 GINA guidelines recommend specialist referral for any child requiring Step 4 care (medium-dose ICS-LABA) or higher, or with any concerning features like frequent exacerbations or diagnostic uncertainty. Collaborate closely with allergists for immunotherapy considerations and pulmonologists for severe cases.
Clear Delineation of Phenotype, Severity, and Exacerbation Management
The Evidence: Severe asthma management has been revolutionized by biologics. However, a 2025 JAMA Pediatrics study revealed significant complexity, showing that 30-40% of children on mepolizumab continued to exacerbate due to alternative inflammatory pathways (e.g., epithelial activation, macrophage-mediated inflammation). This underscores the need for advanced phenotyping.
Specialist Application:
- Provide a Precise Diagnosis: Define the child's asthma phenotype (e.g., allergic, nonallergic, or aspirin-exacerbated respiratory disease [AERD]) and severity classification based on symptoms and lung function.
- Utilize Biomarker-Guided Treatment: For moderate-to-severe cases, use biomarkers (blood eosinophils, IgE, FeNO) to guide therapy, including the selection of biologic agents:
- Omalizumab: For IgE-mediated allergic asthma (age 6+)
- Mepolizumab: For severe eosinophilic asthma (age 6+)
- Dupilumab: For type 2 inflammation with elevated FeNO/eosinophils (age 6+)
- Educate on Exacerbation Recognition: Ensure parents can identify the early warning signs of decompensation, such as increased coughing, decreased activity, or nocturnal awakenings, and know how to escalate therapy according to their action plan.
Integrating Evidence into Specialist Practice
For the sinus and airway specialist, optimizing pediatric asthma care requires a multifaceted, evidence-based approach. It extends beyond pharmacology to encompass validated technique training, comprehensive environmental management, personalized monitoring, and interdisciplinary collaboration. By implementing these strategies—grounded in the latest research on inflammatory pathways and health disparities—we can significantly improve outcomes and safety for our most vulnerable pediatric asthma patients.
To stay current on the latest evidence and collaborative strategies, consider engaging with interdisciplinary networks like the Snot Force Alliance.