Chronic Rhinitis vs. Chronic Sinusitis: How to Differentiate and Treat Effectively
Chronic Rhinitis vs. Chronic Sinusitis: How to Differentiate and Treat Effectively
Every clinician has seen it: patients describing “chronic sinus issues” with months of congestion, drainage, or pressure, only to have the underlying condition misidentified. What’s often labeled as sinusitis is, in fact, chronic rhinitis. This misclassification is common, leading to prolonged morbidity, unnecessary antibiotics, and delayed definitive care.
Despite overlapping symptoms, chronic rhinitis (CR) and chronic rhinosinusitis (CRS) are distinct in anatomy, pathophysiology, and management. This concise guide outlines key distinctions, diagnostic steps, and management protocols— distilled from leading international consensus statements.
Defining the Conditions and Pathophysiology
Chronic Rhinitis (CR)
- Definition: Inflammation confined to the nasal mucosa for more than 12 weeks, characterized by two or more of these symptoms: rhinorrhea, nasal obstruction, sneezing, itching, or postnasal drip [1].
- Pathophysiology: Inflammation is limited to the nasal cavity, primarily driven by:
- Allergic Rhinitis (AR): An IgE-mediated Type I hypersensitivity to aeroallergens triggering mast cell degranulation and the release of histamine, leukotrienes, and cytokines.
- Non-Allergic Rhinitis (NAR): Caused by diverse triggers, including autonomic dysregulation (vasomotor), environmental irritants, hormones, or NARES (non-allergic rhinitis with eosinophilia). Common triggers are temperature shifts, strong odors, and humidity changes.
Chronic Rhinosinusitis (CRS)
- Definition: Per EPOS 2020 guidelines, CRS is diagnosed by the presence of two or more symptoms for more than 12 weeks, one of which must be either:
- Nasal blockage/obstruction/congestion, or
- Anterior/posterior nasal discharge (rhinorrhea) plus facial pain/pressure or reduced sense of smell, and objective evidence of mucosal inflammation [2].
- Pathophysiology: Inflammation extends beyond the nasal mucosa into the paranasal sinuses, driven by:
- Ostiomeatal Complex Obstruction: Blockage of the sinus ostia, impairing mucociliary clearance and leading to stasis.
- Dysbiosis and Biofilms: Disruption of the sinus microbiome and formation of bacterial biofilms that resist treatment.
- Endotypic Drivers: CRS is increasingly categorized by its underlying endotype, primarily Type 2 inflammation (eosinophilic, often with polyps - CRSwNP) and non-Type 2 inflammation (neutrophilic, often without polyps - CRSsNP) [3].
How to Differentiate by Symptoms
While symptom overlap exists, key differentiators can point toward the correct diagnosis.
| Clinical Feature | Chronic Rhinitis | Chronic Sinusitis |
|---|---|---|
| Primary Symptoms | Rhinorrhea, nasal obstruction, sneezing, postnasal drip | Nasal blockage and/or nasal discharge, PLUS facial pain/pressure or reduced sense of smell |
| Facial Pain/Pressure | Rare or mild | A cardinal symptom. Often localized to the maxillary, frontal, or ethmoid regions |
| Smell Dysfunction | Rare, unless due to severe obstruction | A very common and distinguishing feature, especially in CRSwNP |
| Nature of Discharge | Often clear and watery (allergic) or clear/thick (vasomotor) | Typically, mucopurulent (thick, colored). Clear discharge does not rule out CRS |
| Sneezing & Nasal Itch | Very common, especially in allergic rhinitis | Less common |
| Response to Antihistamines / Decongestants | Often good Symptomatic relief | Limited efficacy for core symptoms |
Diagnostic Precision: From Suspicion to Confirmation
Moving from clinical suspicion to objective confirmation is the critical next step.
For Suspected Chronic Rhinitis:
- Anterior Rhinoscopy: May reveal boggy, pale, bluish mucosa (suggestive of allergy) or erythematous, inflamed mucosa (suggestive of non-allergic/irritant).
- Allergy Testing: Skin prick tests or serum-specific IgE are essential to confirm or rule out allergic triggers.
- Nasal Cytology: Scrapings can reveal eosinophils (suggesting NARES or allergy) or neutrophils.
For Suspected Chronic Sinusitis:
- Anterior Rhinoscopy/Endoscopy: This is crucial for objective evidence. Findings may include:
- Mucopurulent discharge from sinus ostia.
- Nasal polyps (typically pale, gray, translucent masses in the middle meatus).
- Mucosal edema or obstruction.
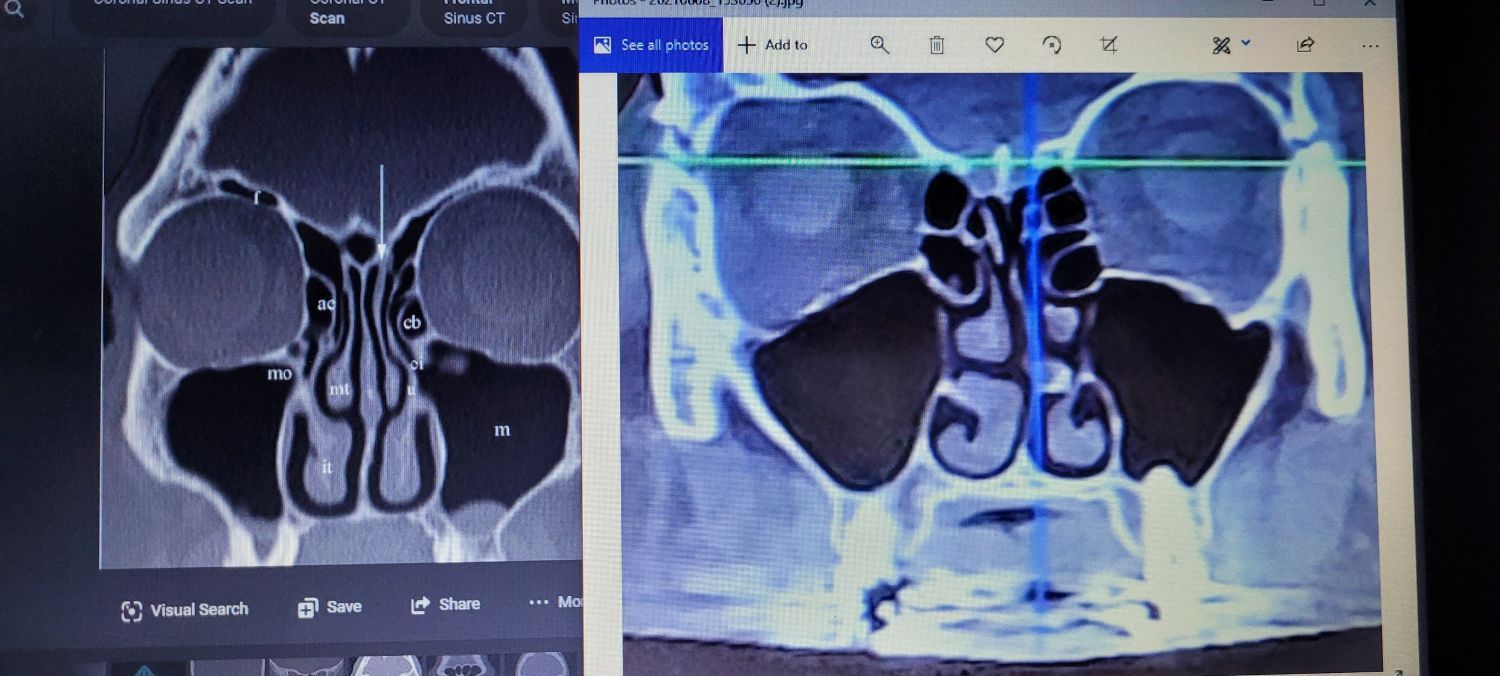
- CT scan of the Sinuses (without contrast): Imaging gold standard. It confirms the diagnosis by showing mucosal thickening, sinus opacification, or ostial obstruction. A CT is indicated when symptoms persist despite medical management or when considering surgery [2].
Treatment Pathways: Tailoring the Approach
Chronic Rhinitis Management:
- First-Line: Allergen avoidance, daily intranasal corticosteroids, and second-generation oral antihistamines
- Second-Line: Adding leukotriene receptor antagonists (for AR), ipratropium bromide (for rhinorrhea), or saline irrigations
- Advanced: For refractory cases, consider referral for immunotherapy (allergy shots or sublingual). In-office procedures like posterior nasal nerve ablation (e.g., with cryotherapy or radiofrequency) have emerged as highly effective for both allergic and non-allergic rhinitis [4]. Intranasal capsaicin is another emerging option for non-allergic rhinitis.
Chronic Sinusitis Management:
- Foundation: High-volume saline irrigations and topical intranasal corticosteroids (including off-label budesonide rinses for post-surgical patients)
- Exacerbation Management: Short courses of oral corticosteroids (especially for CRSwNP) and/or culture-directed antibiotic therapy
- Advanced Medical Therapy: For severe, refractory CRSwNP with Type 2 inflammation, biologics (e.g., dupilumab, omalizumab) are now standard-of-care [3].
- Surgical Intervention: Endoscopic sinus surgery (ESS) is indicated when maximal medical therapy fails. The goal is to restore sinus ventilation and drainage, facilitate topical drug delivery, and remove polyps.
Key Takeaways for the Clinician
- Think Anatomically: Rhinitis is nasal; sinusitis involves the sinuses.
- History is Key: Prioritize the presence of facial pressure/pain and smell loss to suspect CRS.
- Examine the Nose: Nasal endoscopy is a simple, in-office procedure that provides invaluable diagnostic information.
- Confirm Objectively: Use allergy testing for rhinitis and CT imaging for sinusitis when the diagnosis is unclear, or treatment fails.
- Treatment is Condition Specific: Antihistamines are first-line for rhinitis; saline rinses and topical steroids are the cornerstone for both, but sinusitis often requires a more aggressive, multi-modal approach.
By applying this structured framework, physicians can enhance diagnostic accuracy, implement targeted treatment strategies, and improve long-term outcomes for patients suffering from these chronic nasal conditions.
We invite you to join the Snot Force Alliance and take advantage of the resources available to stay informed about the latest findings related to nasal, sinus, and airway conditions. Together, we can improve nasal health and enhance patient care in our practices.
Disclaimer: This blog post is for informational purposes only and should not replace clinical judgment. Always consult the latest clinical guidelines and practice standards.
References
- Wise, S. K., et al. (2018). International Consensus Statement on Allergy and Rhinology: Allergic Rhinitis. International Forum of Allergy & Rhinology, 8(2), 108-352.
- Fokkens, W. J., et al. (2020). European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology, 58(Suppl S29), 1-464.
- Bachert, C., et al. (2020). EUFOREA expert consensus statement on biologics for CRSwNP. Rhinology, 58(4), 311-320.
- Stolovitzky, J. P., et al. (2018). Office-based cryosurgery for the treatment of rhinitis: a prospective, multicenter, randomized, controlled trial. International Forum of Allergy & Rhinology, 8(7), 831-839.