Mastering Airway Evaluation
Mastering Airway Evaluation
In healthcare, few skills are as urgent as managing the airway. It’s the first step in the ABCs of life support. But a truly comprehensive airway evaluation goes beyond pre-intubation checks; it’s a proactive process that can prevent crises before they start.
Whether you’re a nurse, respiratory therapist, paramedic, physician assistant, or physician, this guide will help you evaluate the airway from the nose to the lungs safely and effectively, following established best practices.
Why a "Comprehensive" Evaluation Matters
Think of the airway as a multi-story building.
- The Penthouse (Nose & Mouth): Entry point for air
- The Lobby (Throat & Voice Box): Directs air to the lungs and food to the stomach
- The Main Shaft (Windpipe): Central conduit for airflow
- The Lower Floors (Bronchi & Lungs): Where the real work of gas exchange happens
A problem on any “floor” can cause a system-wide failure. A comprehensive evaluation ensures you identify hidden risks, not just obvious ones at the “front door.”
The Step-by-Step Assessment Framework
1. Patient History - Listen Before You Look
The patient’s history is your first and best diagnostic tool. Key questions to ask (or ask yourself) include:
- Voice Changes? Is their voice hoarse or weak? This can be a sign of a problem at the voice box (larynx).
- Noisy Breathing? Listen for the sound:
- Stridor: A high-pitched, harsh sound. If it is heard when they breathe in, think of the upper airway (larynx). If it’s heard when they breathe out, think about the lower airway (windpipe). If it’s heard during both inhale and exhale, it’s a major red flag.
- Wheezing? A whistling sound often means lower airway narrowing, like in asthma or COPD.
- Trouble Swallowing? Do they cough when they eat or drink? This signals a high risk for aspiration.
- Past Medical History? Previous long-term intubation, tracheostomy, neck surgery, or radiation? These are huge clues pointing toward potential scar tissue or altered anatomy.
2. Physical Exam - Look, Listen, Feel
Move beyond a quick glance in the mouth.
- Look: Check for obvious deformities, swelling, or masses. Look at the patient’s neck—is it short? Is it thick? Do they have a large tongue or a small jaw?
- Listen: Use your stethoscope. Listen over the neck for stridor. Listen to the lungs for wheezes, crackles, or absent breath sounds.
- Feel: Feel the neck for any masses or a deviated trachea ("windpipe") or tenderness.
3. Predicting the Difficult Airway
Anticipating difficult airways is critical to prevent emergencies. Following the ASA Difficult Airway Guidelines, use bedside tools to anticipate challenges:
- Mallampati Score: How much of the back of the throat can you see? (Class I is considered to be an easy intubation; Class IV is considered a hard intubation.)
- Thyromental Distance: The distance from the chin to the neck. Less than three finger-widths can mean a difficult intubation.
- Neck Mobility: Can the patient tilt their head back easily?
If any of these are abnormal, prepare for backup airway strategies, including supraglottic airway devices or surgical airway access.
Your Essential Toolbox
Different tools help us assess different airway regions:
- The Flexible Scope (Nasolaryngoscopy): This is a camera for the throat and voice box. It’s the best way to see if the vocal cords are moving properly and to rule out hidden obstructions. It’s a game-changer for evaluating hoarseness or stridor.
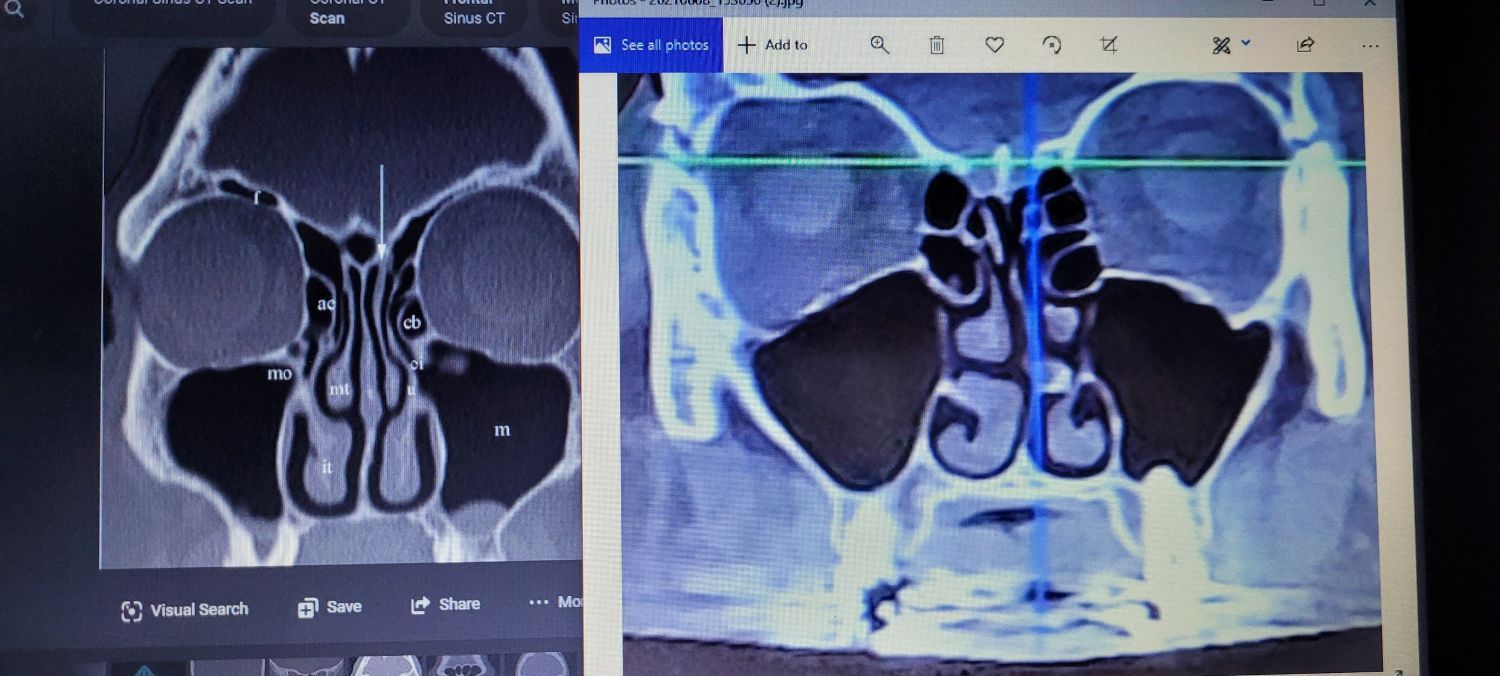
- The X-Ray Vision (CT Scan): This gives us a detailed 3D map of the entire airway, from the voice box down into the lungs. It’s perfect for spotting tumors, narrowing (stenosis), or other structural issues.
- The Functional Test (Pulmonary Function Tests - PFTs): This isn’t a picture; it’s a performance report. It tells us how well the lungs are working—if the patient has obstruction (like COPD) or restriction (like fibrosis).
- The Direct Inspection (Bronchoscopy): This is sending a camera down into the airways. It allows for direct visualization, taking samples (biopsies), and even treating problems like removing a foreign body.
Special Situations to Keep in Mind
- Kids: Their airways are smaller, softer, and shaped differently. A little swelling goes a long way. They require specialized knowledge and equipment.
- Older Adults: They may have less muscle tone, stiffer joints, and more comorbidities, making airway management trickier.
- The Trauma Patient: Assume the worst. Look for facial fractures, neck injuries, and bleeding that could compromise the airway at any moment.
Putting It All Together: The Master Clinician's Mindset
Mastering airway evaluation isn’t about a single skill; it’s about a mindset.
- Be Proactive, Not Reactive. Your goal is to identify the potential for trouble before the patient is in crisis.
- Think Top to Bottom. Don’t stop at the throat. A patient in respiratory distress could have a laryngeal problem, a severe asthma attack, or a pulmonary embolism.
- Use Your Team. You are not alone. Respiratory therapists are experts in lower airway management. Anesthesiologists and ENT (Ear, Nose, & Throat) surgeons are specialists in difficult airways. Use them as early as possible.
- Always Have a Plan B (and C). What if you can’t intubate? What if you can’t ventilate? Knowing your backup options—like using a supraglottic airway or preparing for a surgical airway—is the true mark of mastery.
The Bottom Line: A comprehensive airway evaluation is a blend of careful listening, a structured physical exam, and knowing when and how to use advanced tools. By systematically checking every 'floor' of the airway, you can provide safer care, make better decisions, and be prepared for whatever comes through the door.
This guide is intended for educational purposes to promote interdisciplinary understanding. Always follow your institution's protocols and consult with supervising physicians or specialists as needed.
The Snot Force Alliance is dedicated to disseminating knowledge across relevant medical disciplines and fostering innovation in the medical and surgical management of airway inflammatory diseases. Our goal is to enhance collaboration among various medical fields to improve patient outcomes and advance best practices in treatment.