Understanding the Link Between Sinus Health and Immune Function
Otolaryngology and immunology cross paths frequently, especially when considering the intricate relationship between sinus health and immune function. In this blog, we’ll discuss the connection between these two systems and how they impact an individual's health.
Significance of Sinus Health
Sinus health extends beyond respiratory comfort, serving as a component of the immune system's defense mechanisms. Acting as a protective barrier, the paranasal sinuses filter out pathogens and assist in immune responses. Disruptions in sinus health can compromise this defense mechanism, potentially heightening susceptibility to infections and immune-related disorders.
Implications for Immune Function
Chronic sinus issues can trigger immune dysregulation, affecting the body's ability to fight off infections and maintain overall health. Persistent inflammation can lead to an excessive production of pro-inflammatory cytokines, potentially suppressing immune response and increasing the risk of infections. Understanding this mechanism enables healthcare providers to offer comprehensive care to patients presenting with sinus-related concerns.
Clinical Implications and Management Strategies
Healthcare professionals encounter diagnostic challenges when addressing sinus and immune-related issues due to overlapping symptoms and complexities. By adopting a multidisciplinary approach that integrates insights from otolaryngology and immunology, practitioners can tailor treatment plans that target the root cause of the problem and improve patient outcomes.
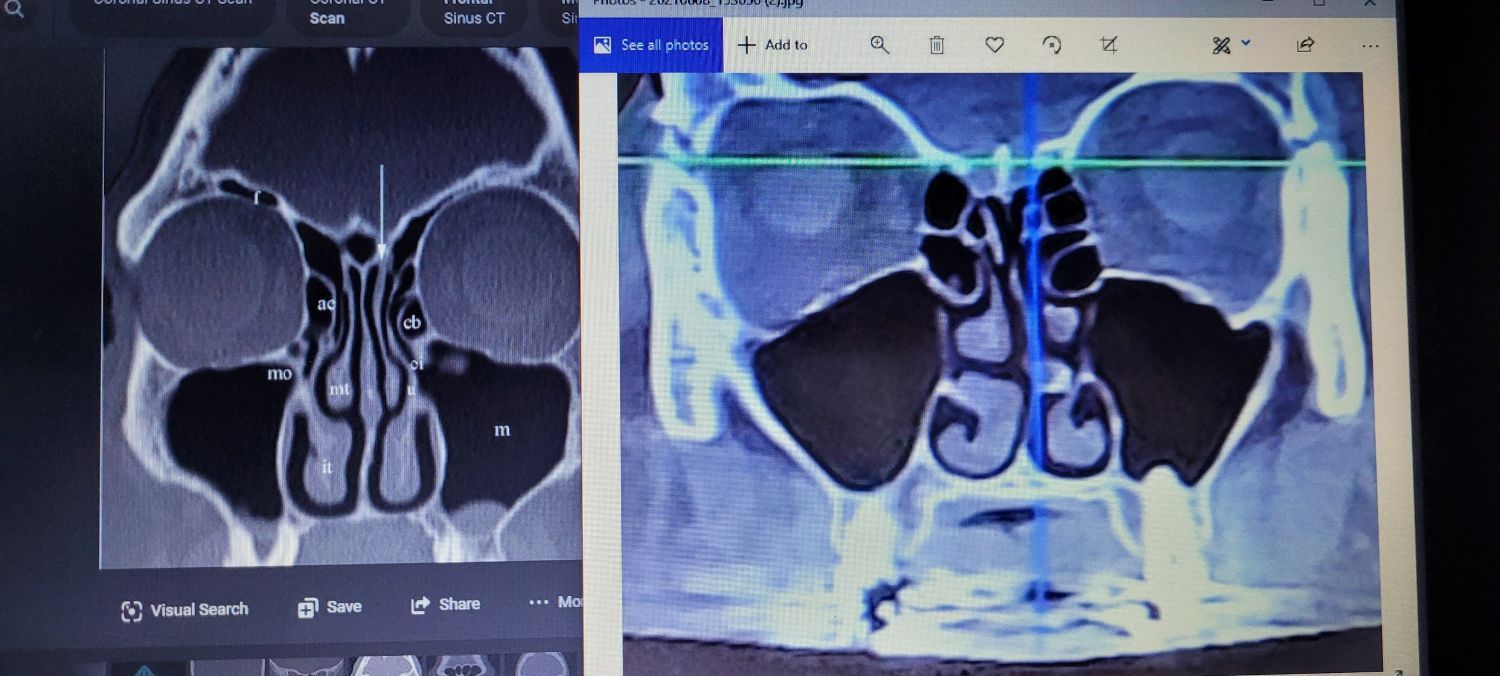
- Diagnostic Considerations: Evaluating patients with recurrent infections or chronic sinus issues necessitates assessing the impact of sinus health on immune function. Utilizing imaging studies or endoscopic evaluations can offer valuable insights into sinus health.
- Treatment Approaches: In addition to incorporating sinus-specific interventions, it is crucial to address underlying conditions such as allergies or structural abnormalities for comprehensive care.
- Collaborative Care: Collaboration among healthcare professionals is pivotal in navigating the complex interplay between sinus health and immune function. By sharing knowledge and best practices, healthcare teams can provide holistic care that addresses both symptoms and underlying immune factors.
- Patient Education: Educating patients on the link between sinus health and immune function can improve treatment adherence and outcomes. Encouraging practices that support sinus health, such as good hygiene, hydration, and allergy management, empower patients to take charge of their well-being.
Snot Force Promotes Interdisciplinary Assessment Approach
Snot Force Alliance is dedicated to advancing interdisciplinary assessment by uniting physicians to collaborate and enhance treatment outcomes. Their webinars and KY Bourbon+Roses Symposium offer a unique platform for participants to broaden their understanding, share insights, and establish meaningful relationships.

Join the Snot Force Alliance to engage in in-depth discussions on all aspects of sinus health and immune function. Become a member today and contribute to driving progress!